Facial Reconstructive Surgery
Facial Reconstructive Surgery
Trauma, surgery or illness can affect the face, both in appearance and function. Many times when a disease was treated, or a patient has survived an accident, residual functional and esthetic considerations require further medical attention. In other cases, the need for immediate facial reconstruction is a part of the overall treatment plan, and it is performed simultaneously.
Our Facial Surgeons have the training, the experience and expertise to reconstruct facial structures, to improve the appearance and restore the functionality of the facial organs. From a simple scar revision to a complex trauma or cancer defect reconstruction, we utilize the most updated techniques and technology to provide natural appearance and function.
The group of our experts works as a team and collaborates with other specialists to provide the best possible result for each patient.
Facial reconstructive surgery generally involves the following categories:
FREE VASCULARIZED TISSUE TRANSFERS
The facial reconstructive surgeons of our clinic were trained in microsurgery. In cases of soft tissue loss, bone loss, or both, they can obtain a graft from other parts of the body along with a feeding artery and two draining veins. The graft is transferred to the area of the deficit and sutured to the tissue bed, while the artery and veins are connected to local vessels with the use of a surgical microscope. By establishing its connection to the systemic circulation, the graft is perfused immediately, so its vitality is ensured. This technique is utilized for a large amount of tissue loss, or when it is evaluated as a preferred option compared to other reconstructive procedures.
The United Kingdom National Multidisciplinary Guidelines regarding head and neck cancer, published in 2016, include the following recommendations for reconstruction following ablative surgery:
- Microsurgical free flap reconstruction should be the primary reconstructive option for most defects of the head and neck that need tissue transfer.
- Free flaps should be offered as the first choice of reconstruction for all patients needing circumferential pharyngoesophageal reconstruction.
- Free flap reconstruction should be offered for patients with class III or higher defects of the maxilla
- Composite free tissue transfer should be offered as the first choice to all patients needing mandibular reconstruction.
- Patients undergoing salvage total laryngectomy should be offered vascularized flap reconstruction to reduce pharyngocutaneous fistula rates.
Free tissue transfer has become popular in many centers around the world. The advantages include aesthetic and functional outcomes, stable wound coverage, minimal donor site morbidity, and the ability to utilize vascularized tissue from remote parts of the body that are outside the zone of injury (trauma, malignancy, infection, irradiation, etc.).
The success rate of this technique is above 90% among experienced surgeons.
Specific donor tissues vary according to the recipient site requirements. The possible donor sites for head and neck reconstruction are:
Radial forearm flaps
Fibula flaps
Anterolateral thigh flaps
Lateral arm flaps
Ulnar flaps
Scapular flaps
Iliac crest flaps
Rectus abdominis muscle flaps
Groin flaps
Dorsalis pedis flaps
Jejunum flaps
Gastroomental flaps
- Innervated muscle flaps are used for facial reanimation procedures.
- Musculocutaneous free flaps are used for large defects requiring aesthetic contouring.
- Fasciocutaneous flaps provide excellent contouring of the head and neck.
- Osseous and osteocutaneous free flaps are useful for segmental bone defects involving the mandible and maxilla.
- Adipocutaneous or perforator flaps are especially useful to minimize donor site morbidity.
- Free tissue transfer is recommended for the irradiated wound, having sown very good results.
A thorough evaluation of the patient’s overall medical condition, the certain anatomic demands of the recipient site and the appropriateness of the donor site must be carefully assessed.
The surgical procedures of this kind are lengthy, especially when combined with the surgical removal of a malignant lesion at the same time.
The patient is admitted for 48 hours to the ICU for close monitoring.
The vitality of the flap is checked every three hours by the surgeons, during the first postoperative day.
Vascularized flaps are considered today the most advanced type of reconstructive surgery.
The rewarding results regarding function and appearance outweigh the physical effort required to perform surgical reconstructions of free tissue transfers.
LOCAL FLAPS, REGIONAL FLAPS
Flap reconstruction is a surgical technique where a type of tissue is lifted from a donor site and moved to a recipient site with an intact blood supply. The flap remains connected to the donor area, and it is primarily used to fill a defect of the skin or the mucosa after the excision of a lesion, in cases of post-traumatic defects, or when correction of a hypertrophic scar is attempted. The difference with a graft is that a flap retains its blood supply from the donor site whereas in grafts the success of the reconstruction is depended on the formation of new blood vessels from the recipient tissue bed to the graft.
Flaps used in head and neck reconstruction can be classified in local and regional.
Local flaps are created by lifting a layer of skin or mucosa and then moving the freed tissue to cover a defect. It is a simple type of flap including the subtypes advancement flaps, rotation flaps, and transposition flaps. When using an advancement flap, the incisions are extended parallel to the wound. A tissue rectangle is formed having one of its sides connected to the donor tissue bed. This side provides the blood supply to the flap. The other three sides of the rectangle are lifted from the underline tissues and then advanced forward to close the wound. The rotation flap follows the same principles except the fact that it is advanced by making an arc, instead of moving it forward. The transposition flap creates an additional defect at the donor area which must also be closed. The flap is moved about the pedicle and transposed over the intervening tissue into the defect. Examples include mucosal flaps, lingual flaps, palatal flaps, rhomboid flaps, bilobed flaps, V-Y flaps, Z-plasty Flaps and many more.
Regional or interpolation flaps are those in which the donor site is not close to the defect. The flap is moved over or underneath normal tissue to reach the defect. The blood supply is still connected to the donor site via a pedicle. This pedicle can be removed later on after blood supply from the recipient tissue bed is formed. Examples include the Platysma flap, Nasolabial flaps, Temporalis muscle and fascia flaps, Forehead flaps, Posterior auricular flaps, Cervical rotation-advancement flaps, Sternocleidomastoid muscle flaps, Latissimus dorsi muscle flaps, Pectoralis major muscle flaps, trapezius flap et all.
The choice between numerous different types of reconstruction is depended upon the specific considerations of each case and the experience of the surgeon. Although it is true that the same defect may be reconstructed in different ways, the esthetic and functional result will justify the choice. The extensive training, experience, expertise and surgical skills of our clinic’s Facial Surgeons could ensure our patients that the best possible effort will be made to correct any esthetic or functional problem in cases of facial reconstruction.
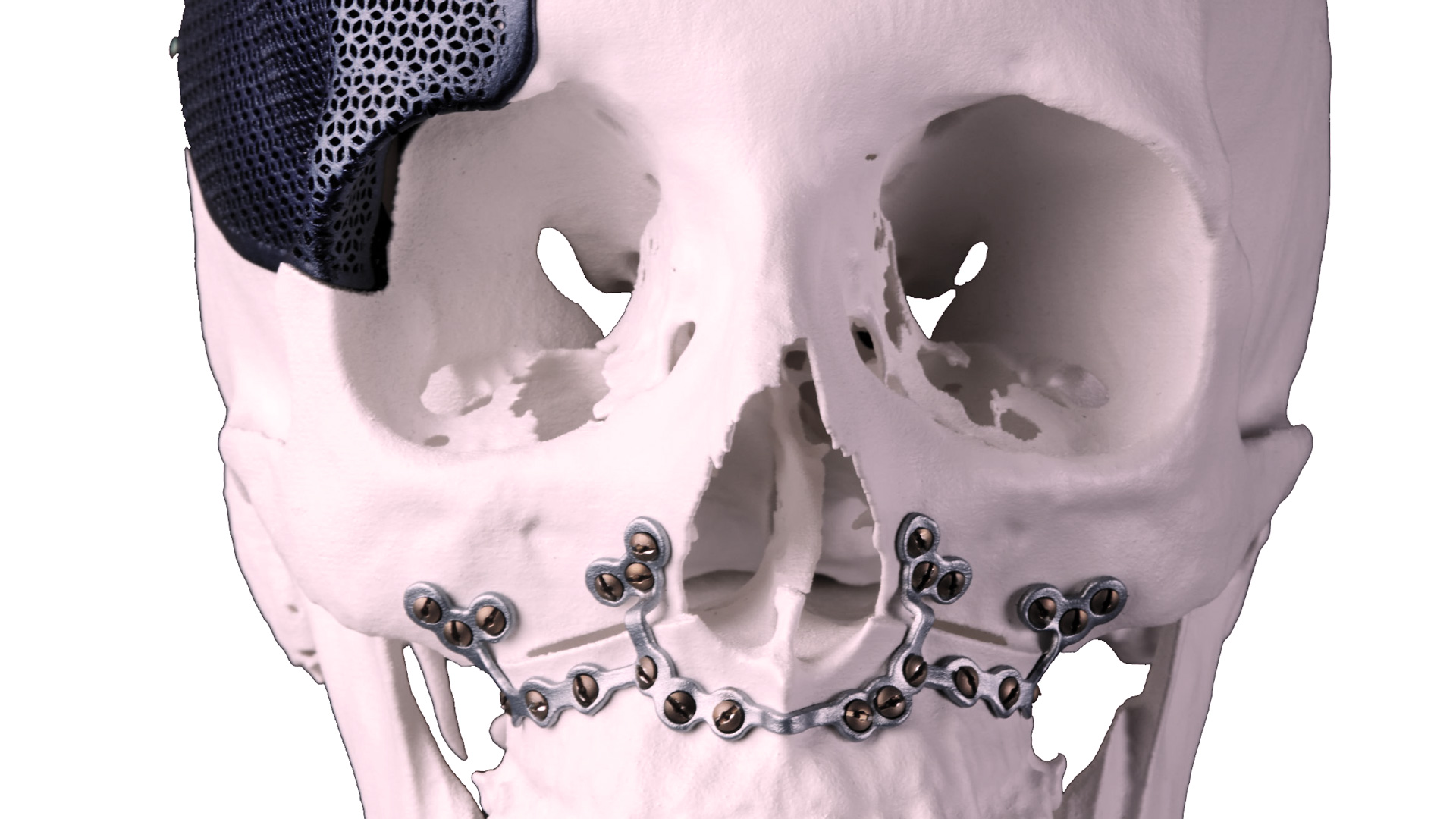
BONE GRAFTS
In cases of remaining bony defects after the surgical removal of intraosseous lesions, as well as when dealing with bony atrophy or skeletal asymmetry, the surgeon may decide to transplant bony tissue from other parts of the body to reconstruct accordingly.
Each case is carefully evaluated regarding the recipient site deficit and the donor site availability. The idea is to transfer a volume of bone cells to the area of interest, to augment its size or to restore its bony deficit. Autotransplantation remains the gold standard of reconstruction in the treatment of bony defects.
Bone grafts may be utilized in cases of:
A post-traumatic bony deficit
After surgical removal of an upper or lower jaw lesion.
In cases of upper or lower jaw atrophy.
In cases of bone loss due to a severe infection.
In some cases of skeletal asymmetry.
In some cases of temporomandibular joint reconstruction
Bone can be transferred in forms of blocs or chips depending on the type of reconstruction. Then they are secured in place with plates and screws, titanium mesh or membranes.
The most common donor sites include:
The posterior area of the lower jaw
The front area of the lower jaw
The posterior area of the upper jaw
The anterior iliac crest
The posterior iliac crest
The tibia bone
The ribs
The calvarial bone
Many times the surgeon will utilize additional treatment modalities to facilitate healing of the bone graft, such as the application of growth factors to the grafted area, in the form of platelet-rich plasma.
The surgeon will explain all associated risks and benefits of the planned procedure.
By applying the relevant surgical principals and implementing the recommended protocols of treatment, bone grafting is a superior reconstructive technique regarding predictability and success.
SKIN GRAFTS
Skin grafting is the transplantation of skin and, occasionally, other underlying tissue types to another location of the body.
The technique plays a role in facial reconstruction when primary closure or second-intention healing would produce a suboptimal result, as well as in cases that local skin flaps are inappropriate, unavailable or would provide an inferior esthetic outcome.
Skin grafts are divided into two major categories: full-thickness skin grafts (FTSGs) and split-thickness skin grafts (STSGs).
STSGs may be subdivided into thin (0.008- to 0.012-mm), medium (0.012- to 0.018-mm), and thick (0.018- to 0.030-mm) grafts.
The use of skin grafts is indicated in reconstruction after surgical excision of malignancies, although skin grafting has several other applications in cases of burns or other skin defects like ulcers.
The choice between the various types of skin grafts depends on many factors such as the size and location of the defect, the esthetic demands of the grafted area, the condition of the adjacent tissues, the underlying pathology which was treated, the training, experience, and preference of the surgeon.
Usually, the surgeon will harvest a part of the skin from selected donor sites and transfer the skin piece to the recipient area. The graft is secured with stitches and dressings or gently pressure gauze bolsters are applied to enchase the healing and avoid hematoma or seroma formation.
In cases of wound contracture or a mismatch in texture and color, laser resurfacing intralesional corticosteroids, dermabrasion or further surgical correction may be implemented for an optimal esthetic result.
ALLOPLASTIC MATERIALS
New technology allows medical professionals to implement biological materials either manufactured completely synthetically or produced by extensive physical or chemical processing of xenogeneic (not species-related) types of tissue.
These materials can play a significant role in the everyday medical practice, as their use may reduce the need for autologous tissues for reconstruction.
We can utilize natural organic and inorganic materials, like materials from animal origin (Collagen, Hydroxyapatite), materials of plant origin (calcium phosphate from algal species), synthetic inorganic materials (tricalcium phosphate), synthetic organic materials (polyglycolic acid), etc
One of the most important applications of new technology is the use of the polyethylene facial implants.
When facial fractures heal in a displaced position, usually a deficit in tissue projection is noted. The same problem occurs when parts of the facial structures (e.g., frontal bone, temporalis muscle) are missing. We will obtain a computed tomogram of the patient’s head, which will be sent to a specialized laboratory for the fabrication of a precise acrylic skull model. We will then study the deficit on this model and sculpt a mold of a custom-made polyethylene graft, to augment the projection of the specific area. As the shape and size of the graft are estimated according to the model, it will perfectly fit the anatomical area of interest during the operation, providing an excellent aesthetic result.
In many cases, we use pre-shaped polyethylene facial implants to augment or esthetically improve areas like the chin, the angles of the lower jaw, the zygomatic bones, the dorsum of the nose, etc. The implant is designed to adapt to its recipient site, it comes in several shapes and sizes and provides an immediate aesthetic result.
Another important alloplastic material we use is the absorbable plating system for the fixation of facial fractures. These plates and screws are made of polyglycolic acid and will be dissolved in a period of six to nine months. The main indication for the use of the absorbable plating system is the growing skeleton (pediatric population). By using this system, we avoid the need of removing a metal plate from a child, because of the anticipated arrest of bony growth that a metal plate would cause. In selected cases, the absorbable plating system may also be used for the adult population as well.
Xenografts like bovine bone can be used to augment the volume of an autologous bone graft, used for facial reconstruction, or correction of upper or lower jaw atrophic areas, before dental implant surgery. We prefer to use autologous bone grafts in all cases, but in some of them we may additionally use the bovine bone xenograft to increase the volume and take advantage if its osteoconductive capabilities.