Dentofacial Deformities
Dentofacial Deformities
According to a classic definition, a dentofacial deformity may present as facial and dental disproportions great enough to significantly affect the individual’s quality of life. An imbalance of the position, the size, and the orientation of the upper and lower jaws may lead to significant esthetic and functional problems.
The causes of these conditions may be inherited, genetic, nongenetic congenital, traumatic, or due to some habits such as sucking of the thumb during early childhood.
We can identify many different types of dentofacial deformities.
- Excessive overjet, (the upper front teeth are in a forward position, relative to a normal occlusion status). This condition can be caused by excessive maxillary growth (where the upper jaw grows beyond the normal facial limits), or deficient mandibular growth (where the lower jaw is posterior to the normal facial limits), or both.
- An underbite, also known as a negative overjet (the lower front teeth are in a forward position, relative to a normal occlusion status), which can be caused by deficient maxillary growth or excessive mandibular growth, or both.
- An open bite, which is a gap between the upper and lower teeth
- Facial asymmetries or occlusal cants (crooked smile)
- Excessive vertical growth of the upper jaw leading to too much of gum showing (gummy smile)
The diagnostic workup of these conditions is extensive. Both the surgeon and the orthodontist will see the patient in a combined consultation. During the initial visit, a thorough medical and dental history will be obtained. An evaluation of the dental occlusion will be performed along with a basic periodontal inspection. Following that, a complete facial esthetic evaluation (front face analysis and profile analysis) will also be done. A speech examination, including a velopharyngeal and tongue posture evaluation, will be performed. The function of the masticatory muscles, as well as of the temporomandibular joints, will also be recorded. Dental casts will be obtained which will be used for further study of the case. Photographs will also be taken as parts of the initial records.
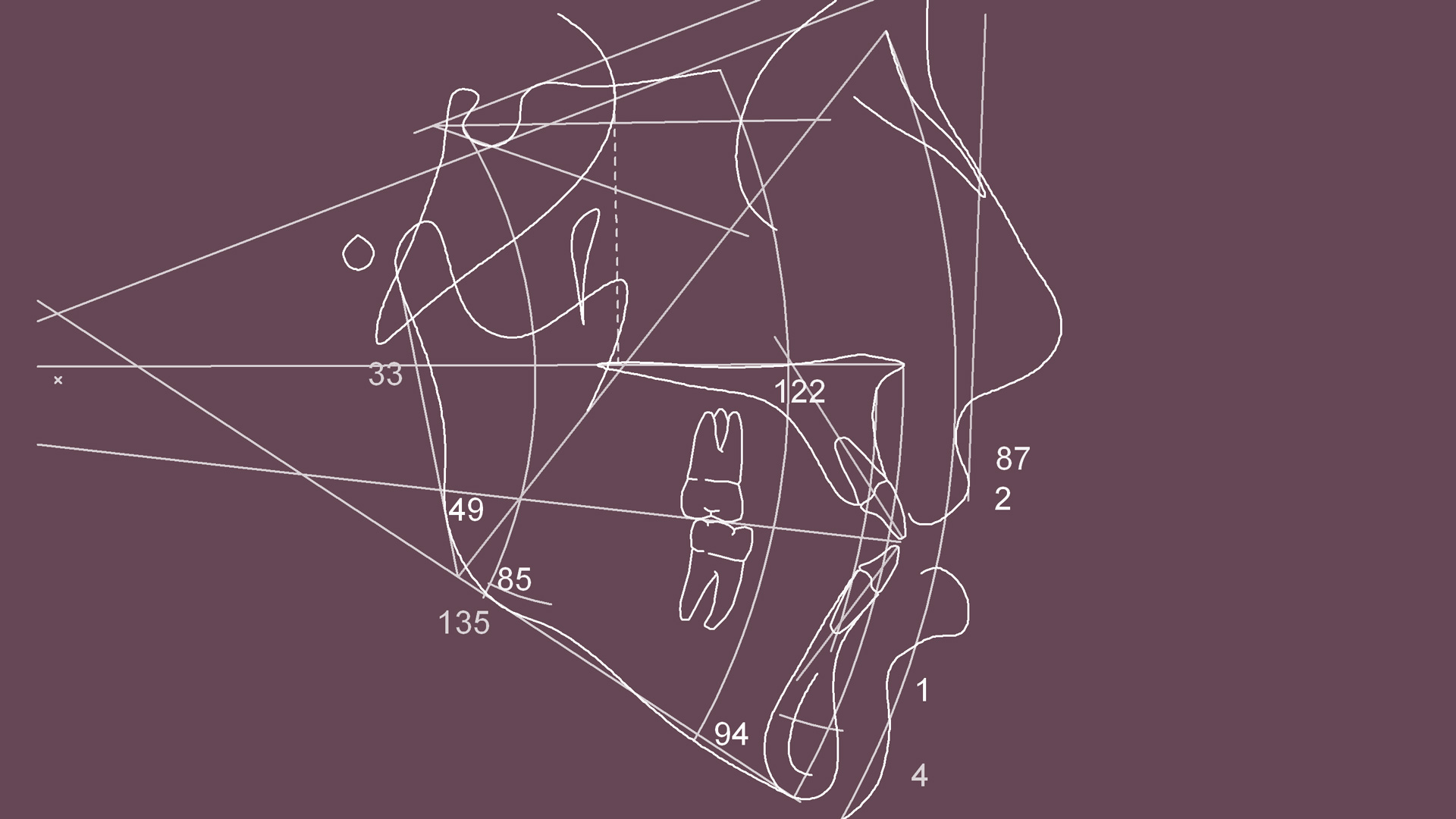
A cephalometric analysis will be made on a lateral cephalometric x-ray. This is one of the most important parts of the preoperative evaluation, as it reveals the imbalances of the facial bones’ position in facial all planes. Sometimes adjunctive radiographic studies may also be necessary such as anteroposterior cephalometric x-rays, radionucleotide scans, three dimensional computed tomographic reconstruction, or temporomandibular joint MRIs. A panoramic x-ray will also be evaluated.
All aspects of the proposed treatment plan will be discussed with the patient. The degree of motivation and the level of expectations from the patient’s part must be assessed. The completion of the treatment is a lengthy process. Therefore it is important to explain all the details and the anticipated difficulties in every step of the proposed treatment plan.
In general, dentofacial deformities are treated by a combined orthodontic and surgical correction. The patient will have to undergo presurgical orthodontic treatment and post-surgical orthodontic corrections. The orthodontist will play a key role in the treatment sequence, as the dental arches will have to be aligned and leveled so that a functional occlusion will be achieved after the surgical correction of the deformity. On the other hand, the surgeon will correct the imbalances in the relation of the facial bones, by moving the upper, the lower, or both jaws into the proper position.
The steps of treatment for a patient with a dentofacial deformity are:
Pre-surgical orthodontics. During this phase, the orthodontist will place braces on the teeth of both the upper and lower dental arches. The teeth will be aligned and leveled to the appropriate position, which ensures that the upper and lower teeth will fit together after the prospective surgical correction of the jaw(s) position.
Surgical treatment (Orthognathic surgery). When the dental arches are set to the desired configuration, the surgical phase of the treatment will be performed. These procedures are carried out under general anesthesia. The surgeon will move the jaw(s) into the appropriate position, and the facial imbalance will be corrected. Post-surgical orthodontics. The orthodontist will correct any minor imperfections regarding the overall position of the teeth to achieve a functional and stable post-surgical dental occlusion.
Post-surgical orthodontics. The orthodontist will correct any minor imperfections regarding the overall position of the teeth to achieve a functional and stable post-surgical dental occlusion.
Q/A GENERAL QUESTIONS
1. I have crooked teeth. Does this mean that I have a facial deformity?
No, not necessarily. People with crooked teeth who do not have signs of facial bone imbalance do not fall into the category of patients with a dentofacial deformity. These patients have a normal projection of their facial bones and require only orthodontic treatment. On the other hand, most of the dentofacial deformities will manifest combined with a type of occlusal imbalance. The orthodontist will easily determine if a case of crooked teeth requires simple orthodontic treatment, or it is a manifestation of a bony deformity as well.
2. How can I tell that I have a facial imbalance?
Some clinical signs may make you wonder whether there is an imbalance in the relation of your facial bones. In different conditions we may receive a positive answer to some of the following questions; a fact that may indicate facial bone imbalances.
“Is your lower jaw too much forward relative to your upper jaw”?
“Is your lower jaw too much backward”?
“Do you think you have a weak chin”?
“Are your cheekbones too hollow”?
“Do you think you have a concave profile”?
“Do you think you have a convex profile”?
“Is your smile crooked”?
“Are your upper gums too visible when you smile”?
“Is your neck-chin angle not very well defined”?
“Do you think that your face is too long”?
“Is there a distance between your front upper and lower teeth when you bite”?
“Is there a gap between your upper and lower teeth when you bite”?
“Do you think that you chin midline deviates to the left or right”?
“Are you unable to freely make your lips touch”?
If you think you have a positive answer to any of the questions mentioned above, you may have to seek a consultation with a specialized facial surgeon who will determine the exact nature of your condition.
3. Am I a candidate for treatment?
Surgical correction of a facial deformity is an elective procedure. Healthy individuals will be able to tolerate the surgical process very well, and the surgery itself will not affect the patients’ overall health status. Rarely, medically compromised patients may not be good candidates for surgical interventions of this kind, as the procedures may not be indicated when health conditions are unfavorable for elective surgeries.
Another important issue is the level of expectations from the patients’ part. Individuals who seek improvement for themselves-not for others are usually excellent patients, who have a realistic and positive attitude towards their treatment. On the other hand, those who are externally motivated, either from their environment, their close friends, their loved ones, may have unrealistic expectations and may be unhappy with the results.
It is important to note that realizing the problem and seeking its correction must be a self-motivating process. It is not advisable to go through an extensive treatment sequence to make other people happy.
We have to make ourselves happy.
It is the surgeon’s responsibility to distinguish between these two types of motivation.
In cases of externally motivated patients, the surgeon has to evaluate carefully whether the patient’s expectations are possible to be met, before the initiation of any treatment.
4. Am I too old to have this kind of treatment?
It is preferable for the patient to undergo a procedure of this kind early enough, so that he/she can enjoy the benefits, both in the functional and esthetic aspect, for the rest of his/her life.
We usually perform orthognathic surgeries at adolescence when the growth of the facial bones is completed, or a few years later.
Surgery is also indicated for older patients who have decided to seek treatment at a later stage. Age is definitely not a contraindication for an orthognathic procedure. Healthy, non medically compromised patients of any age, are good candidates for correction of a facial imbalance.
5. Do the insurance companies cover these procedures?
Unfortunately, the insurance companies consider these types of facial deformities as an esthetic problem. The functional aspect is completely overlooked, so insurance does not cover the vast majority of cases. However, we have dealt with few cases that were covered.
Although the rules are not in favor of the patient, the clinic will provide all the necessary documents when a claim for insurance coverage is attempted. These documents mainly describe the functional irregularities related to these conditions, such as mastication, speech, and temporomandibular joint problems.
6. What will the overall cost be?
The overall cost will include the orthodontist’s fees, the surgical fees, the anesthesiology fees, and the hospital fees. Each case is individually charged, as different conditions require different treatment plans. The estimation of the overall costs is estimated and provided before treatment initiation and will not be exceeded for any reason, other than the rare event of an extension of the estimated hospital stay (increase in hospital fees).
Q/A REGARDING THE ORTHODONTIC TREATMENT
1. Why is orthodontic treatment necessary before surgery?
The orthodontic treatment will serve as a preparation for the upper and lower teeth to fit together after the surgery. This process is done like a regular orthodontic treatment, but the goals of the orthodontist are different when preparing a patient for orthognathic surgery. In that sense, the patient may experience a “worsening” of the occlusion during the treatment. This is desirable and deliberate. The orthodontist has to align and level the dental arches, as well as to reverse the dental compensations that are evident. Many times due to the existing skeletal abnormalities, the teeth have moved to compensate for a gap, an underbite or an overbite. When this occurs, the axes and the position of the teeth are not normal. If this condition is not corrected, dental interferences will prevent moving the bones into the estimated new position during the surgical correction of the deformity. The surgeon will have to put the bones in place, but at the same time, the teeth will have to fit also. A stable immediate post-surgical occlusion prevents relapsing and requires only a few postoperative orthodontic adjustments.
In some selected cases. pre-surgical orthodontics may not be required. The patient will have the braces placed, and most of the dental corrections are done after the surgical treatment.
The widely accepted protocols of treatment, though, include pre-surgical orthodontic treatment as a preparation for surgery.
In our clinic, we initiate the treatment of a facial deformity by utilizing pre-surgical orthodontic treatment as the first step of our treatment sequence.
2. How long will the treatment take?
This is a question asked very frequently. The orthodontist will usually provide a range of time necessary for the pre-surgical preparation of the dental arches and further give an estimation of the post-surgical orthodontic treatment. Many factors and variable conditions will affect the time to complete the above phases. The age of the patient, the density of the bone, angulations of the teeth, the periodontal condition, the surgical plan and the cooperation of the patient, to name but a few.
The goal is to achieve a stable occlusion that will correct the functional and aesthetic issues of each patient. As all the treatments of dentofacial deformities are lengthy and technique sensitive, the orthodontist must be given the time to achieve the best possible result without having to expedite the treatment process, against the quality of the anticipated results.
3. Will I experience discomfort or pain during pre-surgical orthodontic treatment?
Orthodontic treatment uses certain appliances to move your teeth with gentle pressure. When braces are put in place, and after every subsequent visit during activation, you may feel some discomfort. Your teeth and gums may initially feel a bit tender, but usually, this only lasts from around 36 to 48 hours. The degree of the discomfort varies in between patients from minimal to mild and, if necessary, an over the counter pain killer will relieve the symptoms.
4. What is expected of me during orthodontic treatment?
You are expected to keep your appointments because the orthodontic appliances will require periodic adjustments (activation) to be effective. The orthodontist will give you some instructions of oral hygiene that you should follow. You must avoid hard food and sweets. You should keep in mind that pre-surgical orthodontics has a different goal compared to conventional orthodontic treatment. Once you decide to have the treatment initiated, you must commit to the plan. It would be very difficult for the orthodontist to reverse the occlusal changes when the pre-surgical orthodontic treatment is completed if you decide against surgery.
5. Do I keep the braces on after the surgery?
Yes, you will have to keep the braces on for few months after surgery. It is necessary for the orthodontist to make final adjustments of the occlusion so that the best possible final result will be achieved. Sometimes elastic bands have to be used post-surgically to “guide” the dental arches towards a certain position, to avoid relapse and stabilize the surgical result.
6. Can I avoid surgery and have the problem corrected with just orthodontic treatment?
In general, the answer is no. A skeletal problem cannot be corrected by moving the teeth. In some cases, if minor imbalances of the bones are noted, orthodontic treatment may be able to mask the problem. We always take into account the effort to benefit ratio. To propose a surgical correction, we have to be dealing with cases that the surgical effort will obviously benefit the patient. Usually, surgical treatment is decided when the jaw bones have to be rearranged because of a considerable facial imbalance. We do not advise the patients to undergo a surgical correction when the preoperative analysis reveals a discrepancy of a couple of millimeters compared to the normal position of the bone(s).
Q/A REGARDING THE SURGICAL CORRECTION
1. How exactly does the surgeon correct the facial imbalances?
The facial bones will be placed in the pre-estimated position by making certain surgical bone-cuts, and by repositioning the bone(s) to correct the facial imbalance.
Before we analyze the surgical procedure we have to mention the following:
In every case, the dissection and cuts are performed INTRAORALY. There will never be a surgical incision visible on the face. A competent facial surgeon can reach almost every area, below the level of the eye sockets, through the mouth.
Unlike was done in the past, the mouth will not be fixated after surgery. Elastic bands may be placed, in some cases, to guide the occlusion but these are not eliminating mouth opening. It is very rare nowadays that the patient will require wiring of the jaws together.
The accurate positioning of the bones is facilitated with the aid of a prefabricated surgical splint. Suppose, for example, that to correct a facial deformity we have decided to move the upper jaw 7mm forward and at the same time reduce its vertical height by 5mm on the right side and 3mm on the left side. How are we able to estimate the accuracy of this complex repositioning during the operation? The answer is, with the use of a surgical splint. We will place the presurgical dental casts of the patient’s jaws in an articulator (a device that can reproduce the current occlusion by mounting the cast of the upper and lower jaws). Then we will perform all the estimated changes in the positioning of the bones, according to our initial treatment plan and the cephalometric analysis. We will make the cuts on the casts and move the part of the casts which includes the dental arches to the desired position. We measure with every detail that the estimated move has been accomplished in every facial plane. Then on that final position, we fabricate an acrylic splint that we use during the surgical procedure. This splint serves as a great tool in moving the jaws into the correct position intraoperatively. The teeth of the upper and lower jaw will fit within the splint only when the bones have been moved exactly as they were moved on the articulator.
The three most common types of procedures performed in Orthognathic surgery are:
The maxillary Le-Fort I osteotomy. This procedure is done when we have decided to change the position of the upper jaw. It is widely used in cases of a deficient middle third of the face, or when a patient is showing too much of the gums when smiling (vertical maxillary excess), when the smile is crooked, when an open bite exists, and more. The surgeon will make an incision above your upper teeth and then a dissection of the soft tissues until the osteotomy site is fully visible. Following that, the upper jaw will be cut, at a level beginning slightly higher to the base of your nose and moving posterior to the area above your upper wisdom teeth, on both sides. After the cuts are completed the surgeon will detach the upper jaw from its original position and move it to the desired position with the use of the surgical splint. In this final position, the upper jaw will be fixated with titanium plates and screws. This procedure usually takes 2.5-3 hours to be completed.
The bilateral sagittal split osteotomy. This procedure is done when we have decided to correct the position of the lower jaw. It is used in cases of a protruded lower jaw, a deficient lower jaw, a deviated lower jaw, a crooked smile, an open bite and more. The surgeon will make an incision in the area of your lower wisdom teeth on both sides. After the reflection of the soft tissues, bony cuts are made so that the lower jaw is sliced in two pieces on the sagittal plane. By doing this surgical maneuver, the lower jaw will be separated into three pieces; one distal unit, containing the dental arch and two proximal segments containing the condyles and the rami of the lower jaw. The surgeon will then reposition the distal unit into the desired position and then fixate the distal to the proximal units on both sides, with titanium plates and screws or just screws. This procedure usually takes 2-2.5 hours to be completed.
The anterior mandibular osteotomy. This procedure is a useful adjunct to the above procedures, or it can be used as a sole treatment. In cases that the problem involves only the chin area, or when repositioning of the lower jaw is not sufficient to correct an imbalance of the lower third of the face, the anterior mandibular osteotomy is performed. The surgeon will make an incision below your front lower teeth and dissect the soft tissues to visualize the bone. Following that a bony cut will be made, so that the lower part of your chin will be detached from the rest of the lower jaw bone. This segment is then moved forward or backward; its vertical height can be reduced or increased (with the use of a bone graft in between). When the segment is placed in the desired position, it is fixated with plates and screws. This procedure usually takes less than two hours to be completed.
Apart from these basic surgical procedures, many more are included in what is considered as an orthognathic surgical intervention. Surgically assisted rapid palatal expansion, vertical mandibular ramus osteotomies, inverted -L- osteotomies, segmental osteotomies, etc. The specific details and needs of each case, along with the surgeon’s preference and experience will determine the type of the surgical procedure chosen for each patient.
2. What will I experience when in the hospital?
Our office staff will arrange with you the date, the time and all further details of your hospital admission. Usually, we admit the patients the day of the surgery, early in the morning. You just have to go to the admission office and give your name and your social security details. Then you will be taken for the necessary preoperative laboratory tests (blood drawing), an electrocardiogram and a chest X-ray. A member of the anesthesia team will meet you after the completion of the preoperative screening, to discuss the anesthesia details with you. An intravenous line will be started, and some medications may be given to relax you. In the operating room, you will be asleep before any further action is undertaken. While you are asleep a breathing tube will be placed that will deliver oxygen and anesthesia gases during the case. A tube from your nose to your stomach and a catheter into your bladder may also be placed for the surgery. They will both be removed before you wake up, in the operating room.
After the surgery is over you will be taken to the recovery room. You will be closely monitored by specially trained nurses during the first hour after surgery. When you are sufficiently awake, you will be transferred to your room. Your family will be able to see you at this stage.
You may experience some nausea and vomiting, or dizziness due to anesthesia medications. Postoperative pain is rarely an issue. Swelling will develop 24-48 hours after the surgery. You will be fully covered with anti-nausea medications, antibiotics, medications to control the swelling, medications to protect your stomach, as well as pain medications. Minor bleeding may occur from your nose and mouth, which can be controlled with packing. Nasal stuffiness may also occur which can be managed with a combination of nasal sprays and cleansing of the nostrils. The first day you will start taking clear liquids, and by the time you manage to drink a sufficient amount of fluids, your intravenous fluid intake will be discontinued. You will be encouraged to walk as soon as possible, even few hours after the procedure. You will also be able to talk and communicate with your visitors.
Your overall condition will improve the day after the surgery. When we make sure that you can support yourself at home and there is no need for further hospitalization you will be discharged.
3. How long will I have to stay in the hospital?
When an anterior mandibular osteotomy is performed, the patient will most likely be sent home the same day.
In cases of single jaw surgery (upper or lower), the patients will be discharged the day after their surgery.
Patients who underwent double jaw surgery will usually be discharged after two days.
4. What will I experience after surgery?
At home, you will be initially able to drink, as you did during your hospital stay. You will advance your food intake to soft/pureed diet in few days. You may experience a transient weight loss. When you resume a normal calorie intake, your weight will get back to the preoperative levels. Sometimes drinks high in calories may be prescribed to you to consume during the first week after surgery.
Swelling will peak the third or fourth day after the procedure. It will slowly decrease over the next 7-10 days. A small percentage of residual swelling may be evident for a month.
Pain may be anticipated, but it is easily controlled by orally taken pain medications when necessary. It is very rare to receive a report of excessive pain from one of our orthognathic patients.
You will also have to take antibiotics for one week, nasal decongestants (for upper jaw surgeries) and put some ointment to keep your lips moist. Maintaining good oral hygiene during the postoperative period is necessary. You will be able to brush your teeth immediately after you’re discharged from the hospital, and additionally to use some mouth rinsing solutions.
You will receive special instructions if you were discharged with elastic bands, or you were instructed to keep your surgical splint in place after your surgery. As we closely monitor the patients during the initial postoperative period, follow up visits on a weekly basis will be necessary for the first month postoperatively.
5. When can I resume my regular activities?
You can resume your regular activities two weeks after surgery. The time of resuming your previous activity at work or school is depended on the severity of the surgical correction, on whether the postoperative course is uneventful and on the individualized will of every patient to return to previous activities. The avoidance of contact or aggressive sports is important, though.
Please note that it takes 6 to 8 weeks for initial healing of your jaw(s) and 8 to 12 weeks for complete bony healing. If the jaw is hit early after your surgery, this may cause some shifting in the jaw(s) and alteration of your bite. In this unfortunate event, you may need further surgical intervention.
6. Could I speak to other patients who have had a similar procedure done?
We believe that when former patients share their experience with prospective patients, many of the fears, doubts, or second thoughts, are controlled. In that sense, we encourage new patients to discuss with someone who had a similar procedure done in the past from our group. This discussion is held in private, and the members of our medical team are not present.
You will also be asked if you would like to share your experience, after the completion of your treatment, with a future patient. As the release of contact details of former patients is not permitted, due to regulations regarding sensitive personal data, we can only provide the contact information of those who have signed the relative consent form, allowing their information to be released for this purpose.